- May 22, 2025
- Web Editorial Board
- Health Guide, Treatment Methods and Operations
Cryoablation: Non-Surgical Prostate Cancer Treatment
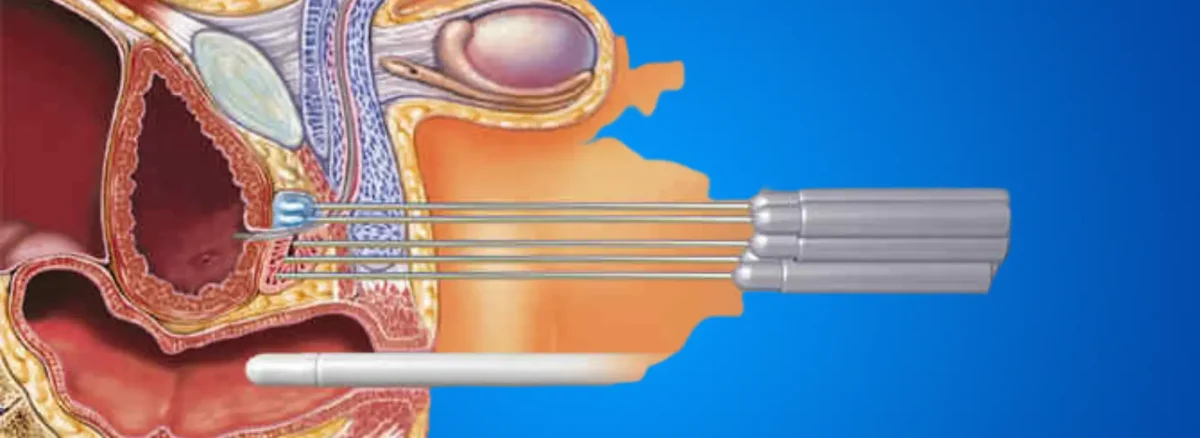
Cryoablation is a minimally invasive treatment method used in cases of localized or recurrent prostate cancer. It works by freezing tumor tissue below -40°C, leading to cell death. In an operating room setting, needle-like cryoprobes are inserted into the prostate, and cancerous cells are targeted through controlled freeze-thaw cycles.
What is prostate cryoablation?
Cryoablation (cryotherapy) involves the formation of ice balls in the targeted tissue using argon or helium gas-cooled probes. This process disrupts the cell membrane and blood vessels of cancerous tissue. Temperature sensors placed around the prostate help protect surrounding tissues (urinary sphincter, rectum).
Who is it suitable for?
- Patients with low to intermediate-risk localized prostate cancer (Gleason ≤ 7, PSA < 20 ng/mL)
- Patients with systemic conditions that contraindicate surgery or who perceive radical prostatectomy as high risk
- Patients with local recurrence after radiotherapy
- Cases where focal cryotherapy is intended to target only the tumor area
How is it performed?
Preparation: The patient is placed in the lithotomy position under spinal or general anesthesia.
Probe Placement: Under transrectal ultrasound guidance, 5–10 cryoprobes are inserted into the cancerous areas of the prostate.
Freeze Cycle: Rapid freezing with argon gas (≈ -140°C) followed by warming with helium gas is applied; two cycles are typically sufficient.
Catheterization and Follow-Up: A urinary catheter is placed at the end of the procedure and is usually removed within 1–2 weeks.
What are the advantages?
Minimally Invasive: No open surgical incision; shorter hospital stay.
Repeatable: Can be repeated or combined with other treatments if needed.
Low Blood Loss: Blood transfusion is rarely required.
Quick Recovery: Return to daily activities is typically within 1–2 weeks.
What are the possible risks and side effects?
- Temporary urinary incontinence or weak urine stream
- Erectile dysfunction
- Perineal pain, swelling, or hematoma
- Rare rectal injury or fistula formation
- Temporary PSA elevations during follow-up
What is the recovery process like?
First 48 hours: Mild perineal pain and blood in urine may occur; fluid intake should be increased.
1–2 weeks: Catheter is removed; return to office work is possible.
4–6 weeks: Gradual return to intense physical activity and sexual life.
3–6 months: Treatment response is assessed with PSA monitoring; MRI or biopsy may rarely be needed.
What are the costs of prostate cryoablation?
The cost varies depending on the hospital’s technical infrastructure, number of probes used, type of anesthesia, and insurance coverage. Please contact us for detailed pricing.
Frequently Asked Questions About Prostate Cryoablation
1- Is prostate cryoablation painful?
The procedure is performed under anesthesia; mild perineal pain afterwards can be managed with analgesics.
2- What is PSA (Prostate-Specific Antigen)?
PSA is a protein produced by the prostate gland, found at very low levels in the blood. It is measured with a simple blood test and is used in screening and monitoring conditions such as benign prostatic hyperplasia (BPH), prostatitis, and prostate cancer.
3- When does PSA level decrease?
A gradual decrease is expected within the first 3–6 months. Near-zero levels are not the target.
4- How long is the urinary catheter kept in place?
In most cases, it is removed after 7–14 days.
5- Is erectile function completely lost?
The risk is low in focal cryotherapy. In whole-gland applications, the risk of erectile dysfunction increases.
6- Can the procedure be repeated?
Yes, it can be repeated in case of local recurrence or combined with other treatments.
7- Is it suitable for recurrence after radiotherapy?
Yes, it is an effective option for selected patients.
8- When can I return to work?
You can return to desk work within 1–2 weeks; for physically demanding jobs, a 4-week wait is recommended.
9- Is urinary incontinence permanent after the procedure?
In most cases, it is temporary. Pelvic floor exercises can speed up recovery.
10- Is the tumor completely eliminated?
Success depends on case selection. In certain lesion sizes, control rates can reach 80–90%.
11- What is the quality of life like after the procedure?
Most patients maintain their quality of life due to low pain, short recovery time, and quick return to daily activities.
References
- Mayo Clinic
- Cleveland Clinic
- Johns Hopkins Medicine
- National Cancer Institute
- American Cancer Society
- Prostate Cancer Foundation
- European Association of Urology
- American Urological Association
- Cancer Research UK
- Urology Care Foundation
- NHS (UK)
- Medscape
- PubMed
- WebMD
- Healthline